A GLOBAL VIEW
A GLOBAL VIEW
To give some perspective on the specific focus of this years’ meeting in Mexico, GRIP members from across the globe were asked to provide an update on current progress and future plans in their local markets.
Professor Dr Attila Altiner
Germany
Although being a low prescribing country “The German government recently provided substantial funding for projects and largerscale educational campaigns to further reduce antimicrobial use”, Dr Altiner explained.
One recent program run by Dr Altiner at the Institute for General Practice, Rostock University Medical Center, sought to test the effectiveness of an intervention known as RESIST (Reducing antibiotic RESISTance through adequate use of antibiotics for acute respiratory tract infections), which set out to reduce the rate of inappropriate antibiotic prescriptions for acute respiratory tract infections (ARTI) in Germany. Centred around providing better physician and patient education around the risks of AMR through e-learning, more than 2,500 General Practitioners took part.
Pharmacy continues to represent an opportunity within Germany, Dr Altiner said. Leading a roundtable discussion and a press meeting at Expopharm, Germany’s largest pharmacy meeting, Dr Altiner championed a greater involvement for pharmacy in Germany with GRIP: “We do a lot of projects with pharmacists. They’re longing to show that they have a responsibility too. In Germany, antimicrobial stewardship could be promoted a lot more in the pharmacy than at present.”
Like other countries in the EU, US and Australia, “the role of pharmacy should be actively considered in Germany”, said Dr Altiner, “and there could be a stronger role for pharmacists, such as providing flu vaccinations”. One major obstacle could be the German health system which might be somewhat resistant to an expanded pharmacy role: “This leaves a situation where the pharmacists are afraid of being in conflict with the conservative doctors’ associations, who are still very strong players in the system. This is a real problem in Germany,” said Dr Altiner.
One solution, he suggested, could be to demonstrate how pharmacies could be effective partners in community-based education, leveraging their ability to talk to many people on a daily basis, and using the power of health literacy.
Dr Altiner shared some health literacy examples from Germany which aimed to educate the public on AMR through the fun medium of a comic book. Students Florian Polte and Ferdinand Boddien developed the comic “Adventure in Immunopolis” in their course at the University of Wismar and it has been made available to the public in GP waiting rooms throughout Germany.
To conclude, Dr Altiner would like to encourage closer working between young pharmacists and doctors in order to tackle the challenge of AMR. He said,
”Bring young doctors and young pharmacists together, because they are some kind of different species and there is so much potential through working together.„
Mr John Bell
Australia
Mr Bell showcased work in New Zealand where a pilot study had been run with Green Cross Health, a pharmacy provider with more than 350 community Pharmacies throughout New Zealand. The study had the aim of the reducing URTI treatment with antibiotics and providing symptomatic relief to meet patients’ needs.
The project centred on empowering pharmacists to provide diagnostic throat swab testing. Patients who tested positive for streptococcal A infection were referred back to the doctor; if the test was negative, patients were offered advice and symptomatic relief.
The pilot study proved to be very successful, chiefly in two areas, said Mr Bell, “Firstly, identifying pharmacists to whom people should go for advice, information and evidence-based products for self-limiting URTI conditions like sore throat; and secondly
helping to convince patients that maybe seeking or expecting an antibiotic, in the first instance, wasn’t the right decision.”
There is still an ongoing discussion around whether to translate the pilot for Australia and other markets, both because of cost and also acceptability to the pharmacy and medical professions; as there remains an issue around whether people should be receiving this kind of service and information from pharmacies rather than doctors.
Nonetheless, the Australian Therapeutic Guidelines had seen fit to publish an addendum to the antibiotic prescribing guidelines in August last year which specifically addressed acute rhinosinusitis, acute otitis media, acute pharyngitis, tonsillitis and acute bronchitis. “For all these conditions, the new guidelines recommend first-line therapy should be symptomatic treatment not antibiotics”, concluded Mr Bell.
Dr Douglas Burgoyne
USA
“Looking at deaths caused by AMR in 2019, the CDC reports that there were about 35,000 and 2.8 million infections. If you include C. difficile the number of course goes up,” Dr Burgoyne said. “However, that’s half the number of 2013. So in the last six years there’s been significant efforts around AMR that is having positive outcomes on mortality. That’s the good news.”
Results also showed that antibiotic utilisation in the primary care setting in the US is improving, with only around 15% of patients who ask for an antibiotic in a physician’s office receiving them.
Pharmacy is also changing in the USA, with
an increase in the
number of
pharmacies offering immunisation and
vaccination,
particularly in patients
over 65. This model is gaining traction
because
the amount the insurance companies need to
pay the
pharmacy is less than they
would need to reimburse the physician’s
office for the same immunisation. This represents valuable additional income for the pharmacists, which makes up for any lost revenue from dispensing, whilst keeping patient satisfaction high.
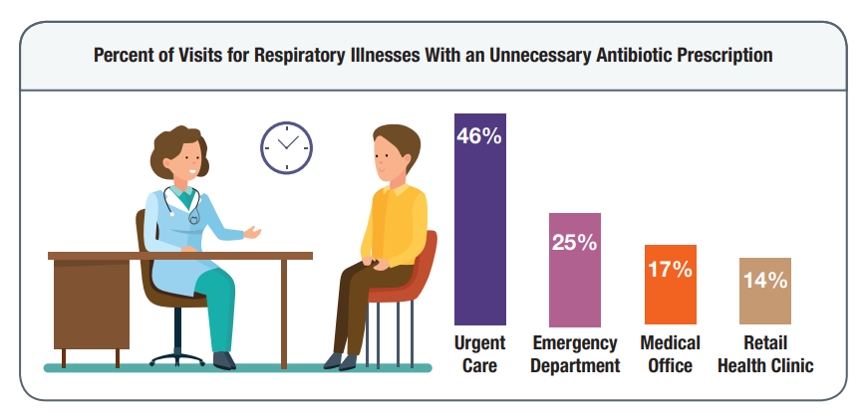
However, Dr Burgoyne went on to caution that there remains concern around the level of inappropriate antibiotic prescribing in the Urgent Care setting in the US. Urgent Care units are standalone physician’s offices that act as a replacement for the ER at a lower cost. “People pay to see a physician and it’s not always covered by insurance, and this often drives patients’ expectations”, he reflected.
There is also work to be done with health insurance companies, he said: “There are still too few health insurance companies engaging their members in AMR. Payers and insurance companies used to look at antibiotics as inexpensive, so they didn’t really care about it because it was cheap. That strategy has changed. More information about quinolones, for example, and the long-term impact on health has influenced payers to start putting a little more regulation and messaging about appropriate use so that’s all good news”.
”As a nation we didn’t really have an antibiotic resistance campaign until 2001, and then we kicked it off. So it’s about 20 years there’s been significant reduction in mortality and improvement in utilisation. So we’re glad about that„
Dr. Martin Duerden
UK
“It’s viewed as critical to the country featuring on the Civil Contingencies Risk Register along with situations like flu epidemics, certainly the Coronavirus epidemic now, flooding, global warming and terrorist attacks.”
A large number of training materials and resources are available from the Royal College of GPs ‘TARGET’ website (Treat Antibiotics Responsibly, Guidance, Education and Tools; https://www.rcgp. org.uk/clinical-and-research/resources/toolkits/amr/targetantibiotics- toolkit.aspx)
Today, AMR and antibiotic prescribing is something that GPs are all measured against, explained Dr Duerden, so they are expected to take audits of their use of antibiotics into their annual appraisals, and those annual appraisals feed into their revalidation. Although it would be highly unlikely that a GP would get removed from the register, Dr Duerden reflected that this is enough of a potential
threat to make a lot of GPs more aware of their prescribing practise.
Public Health England has also campaigned in this area with its initiative, ‘Keep antibiotics working’. Within the UK there is a lot of encouragement to get the public to sign up toantibioticguardian.com and make a pledge to use antibiotics responsibly. “You make a pledge only to take antibiotics if it’s absolutely essential. Which has been quite successful as lots of people know about it now”, stated Dr Duerden.
Dr Duerden also addressed the issue of backup or delayed prescriptions. Admitting to being somewhat of a sceptic to the National Institute for Health and Care Excellence (NICE) guidelines in this area, Dr Duerden referenced a recent Cochrane review looking at 3,700 patients with respiratory tract infections. It showed 93% of patients who were given an immediate prescription got them, whereas delaying a prescription resulted in 31% of people using antibiotics for a respiratory tract infection. The best result was in patients who were not prescribed an antibiotic, where only 14% of patients received a prescription following deterioration of their condition. He said, “My view is that we should go for the don’t prescribe option, and we need to have that big culture change, but within reason. I think maybe it helps if you work within a practice where denying patients is not commonplace.”
Dr Duerden concluded with another big success story in the UK, “MRSA has just about gone away because of hospital hygiene processes and better antibiotic usage”.
Prof. Sabiha Essack
South Africa
South Africa was the first country in Africa to develop its National Action Plan from 2014 to 2024, explained Prof Essack.
With regard to implementation, Prof. Essack explained that like most other countries “we are challenged to secure investment to implement the action plan, and whatever has been done to date has been based on existing programmes in the country”.
Progress was being made in the area of surveillance of antimicrobial use and resistance, Prof Essack said, and while the data wasn’t perfect because it was based on market research data and voluntary laboratory submissions respectively - which tended to overestimate resistance – it was progress.
GRIP activities in South Africa have looked again at pharmacy interventions, and found that the GRIP ‘Flip book’ provided a statistical significant increase in knowledge and awareness amongst the pharmacists.
Prof. Essack ended on a success story, that demonstrates the positive impact when several government departments come together to work towards a One Health Issue. “When the mobile mcr gene was found to confer colistin resistance first in China, we also looked for it in South Africa and it was found in poultry, it was found in pigs, it was found in humans both in hospitals and in communities and in the public and private sector. So like everybody else we also were concerned about making sure that the stewardship of colistin was working well.”
“We worked with the South African Veterinary Council and the South African Health Products Regulatory Authority which is our health products regulator. The human health, animal health and national departments, as well as the drug regulator, worked together to first of all remove colistin as a feed additive. We used to get them in big barrels, that used to be added to water, so it was a big task to completely remove colistin.”
The work resulted in colistin being upscheduled in South Africa, meaning that it had to be on prescription for veterinary purposes and needed special permission from the Department of Health for use in humans, Prof. Essack concluded.
”This was a One Health issue where several different departments came together and worked towards the greater good. That was the colistin success story.„
Prof. Antonio Carlos Pignatari
Brazil
Prof. Pignatari explained that One Health, like in other countries, is a key discussion point for Brazil. It is a relatively new topic and part of the government plan is to work together with Universities, due to grants that are available.
At the national GP Congress in November 2019, information on the GRIP philosophy and associated educational materials were distributed and were well received by the physicians in attendance.
Prof. Pignatari said there remained a great opportunity to work with pharmacists in Brazil. Whilst some barriers exist to empowering this audience and there was tension between a new generation of pharmacists and conservative doctors, Brazil is following the US model and, like other countries, the pharmacist is no longer there to just dispense medication but can discuss a clinical point of view and is the closest HCP to the patient.
Inspired by the GRIP work to date in other countries, connections have been established with the local council of Pharmacy, although local legislation may prohibit any information being distributed to the general public.
However, the future looks bright. Prof. Pignatari concluded that through working with pharmacists on the AMR issue, “there is potential to build a trust relationship with the patient to prompt much needed behaviour change and stewardship in Brazil.”
Dr. Aurelio Sessa
Italy
Italy has one of the most severe challenges with antibiotic prescribing in the EU, explained Dr Sessa. However, the overall daily defined dose (DDD) has reduced by around 10% in Italy – although this remains high by European standards. Not all parts of Italy have the same challenges, Dr Sessa said: “You see a difference from the north to south of Italy. The north of Italy is about the same as the best country in Europe, so we must work a lot with our colleagues in the centre and the south of Italy.”
Whilst results were not available broadly, Dr Sessa highlighted his work in the Lombardy region of Italy to reduce prescribing behaviours.
Firstly, all local antibiotic prescribing data in the primary care setting is shared. This is followed by the sharing of all local data on AMR by the microbiology laboratory. This data is discussed in an audit between small groups of doctors (GPs, family pediatricians, microbiologists, emergency care doctors). The group is then able to provide guidelines and recommendations on the management of conditions such as respiratory tract infections. This process aims to reduce the number of inappropriate antibiotic prescriptions.
To conclude, Dr Sessa talked briefly about the problem with the relationship with the pharmacist in Italy. He said, “We tried to have a programme for education with pharmacists but most pharmacists are conservative and say, It’s not our problem because we don’t prescribe antibiotics”. Furthermore, it is estimated that around 10% of pharmacists in the south of Italy dispense antibiotics without a prescription.
The Medicines Utilisation Monitoring Centre in Italy (OsMed) recently reported that that 80% of antibiotic prescriptions are in the community, said Dr Sessa, which has emphasised the need for attention at a primary care level in terms of surveillance, particularly as most antibiotics prescribed are for respiratory tract infections.
Referencing the Italian National Plan, presented in 2017, this set out objectives to achieve a:
- 10% decrease in antibiotic prescription in the community setting by 2020
- 5% decrease in the hospital setting and 30% in animal breeding by 2020
- 30% decrease of antibiotic prescription in animal breeding by 2020
However, there is some hope as Dr Sessa explained, “In larger pharmacies there is now one doctor that treats so-called minor diseases for the patient; diarrhoea, headache, joint pain, respiratory tract infections etc. and they are aware of the problem posed by AMR. So we hope that with the Society of General Practitioners and the Society of Clinical Pharmacy coming together, we can share the problem of AMR and also improve the relationship with patients”.
Dr Sessa ended on a message given to GPs and specialists in the region,
”Every time we are prescribing an antibiotic we must wonder: it is it really required? Do I have an alternative? This antibiotic that I’m prescribing for my patient, is it right or not?„
Dr. Wirat Tongrod
Thailand
Dr Tongrod opened with an update on the situation in Thailand. He said, “AMR is a major problem because they have had 30,000 deaths due to AMR this year”. A campaign for AMR was started more than ten years ago and around three years ago the prime minister endorsed the Ministry of Health to set a national strategy plan to combat AMR. This strategic plan aimed to reduce deaths by 50% from AMR, and also try to reduce the use of antimicrobials by around 20%.
As part of this strategic plan, Thailand is implementing an action plan specifically for use in hospitals. The government has set Key Performance Indicators to reduce the use of antimicrobials in the hospital, where the problem of AMR is particularly prevalent. These measures are going some way to reducing irrational antibiotic use but it is recognised that an integrated approach is needed across all healthcare sectors.
In community pharmacy, campaigns aim to educate pharmacists and patients together about appropriate antibiotic use. Dr Tongrod has been involved in the development of a toolkit and mobile application that aids dialogue on appropriate antibiotic use between the patient and pharmacist, promoting responsible antibiotic use.
Every year Thailand promotes National Antimicrobial Awareness Week in November, with many public campaigns running during this time. Dr Tongrod shared a campaign video funded by the Thailand health promotion fund which is essentially the tax collected from alcoholic beverages and tobacco. The video was aimed at educating a new generation on AMR, portraying an entertaining bacteria vs virus catwalk fashion event. It was extremely popular, with over 2 million YouTube views.

In Thailand, policy now states that every pharmacy must have a pharmacist on duty, and this will be enforced in phases over the next two years by government. Dr Tongrod commented, “We have tried to implement this law and regulation but it’s not easy, it has taken 50 years to do this”.
Dr Tongrod ended with an update on a Leaders Forum he attended last year, hosted by the Federation of Asian Pharmaceutical Associations (FAPA). FAPA includes membership from the Middle East and South East Asia, as well as the Western Pacific regions encompassing Australia and the Philippines. At the FAPA Summit last year in Bangkok, the role of the pharmacist in immunisation was promoted. Immunisation is commonplace in pharmacies across Australia and the Philippines, but not yet in Thailand. Dr Tongrod sees this as an opportunity for pharmacists in Thailand to feel empowered to prevent AMR and the unnecessary use of antibiotics by reducing the risk of infections through the promotion of immunisation and community health. More information on the FAPA Leaders Forum can be accessed here: http://fapa.asia/2019- fapa-leaders-forum-on-the-roles-of-pharmacists-in-promotingimmunization/
Dr. Alike van der Velden
Netherlands
Dr van der Velden began with an update on a programme initiated 2 years ago by the Dutch Ministry of Health, the National Implementation of antibiotic surveillance & stewardship in primary care. The aim of this programme was to organise and facilitate antibiotic surveillance and stewardship in primary, secondary and long-term care – as well as trying to integrate this care.
Dr van der Velden provided an update on the pilot recently conducted for primary care, which began with defining a new set of informative quality indicators. Each general practice in the pilot was provided with practice-level feedback on the outcomes of the quality indicators during an educational session. The new quality indicators included measures such as the number of antibiotics prescribed per 1,000 registered patients, revealing unexpectedly large variation in antibiotic prescribing quantity between the various practices measured so far.
An evaluation of this programme reported that 88% of participants expressed a great need for new added value quality indicators and 91% regarded that the new indicators were useful or very useful. In particular, GPs appreciated the quality indicators linked to the current prescribing for pneumonia, upper RTI, urinary tract infection and otitis media. Based on this feedback, Dr van der Velden and the team concluded that the new quality indicators and associated education was a good approach to improve antibiotic prescribing behaviour.
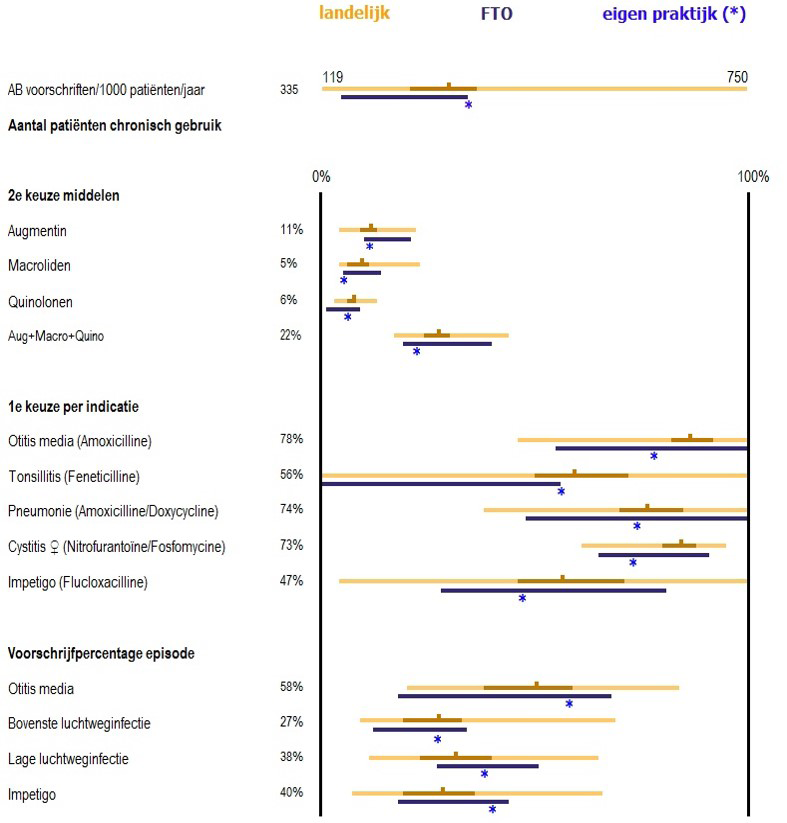
Moving on to talking about surveillance more generally in the Netherlands, Dr van der Velden explained that the Ministry has divided the Netherlands into ten regions, and each region has a team composed of representatives from primary, secondary and long-term care and public health, to design and implement programmes in their regions which they think are necessary for antibiotic surveillance and stewardship. They have all received a budget of €1 million for four years and have to organise actions around reducing inappropriate antibiotic use, delaying development and spread of resistance, reducing preventable healthcare infections
and early detection. The programme developed for Primary Care is known as SABEL, which stands for Mirror Antibiotic Prescribing Quality in Primary Care.
Dr van der Velden and her team have now implemented their own SABEL programmes in two regions, reaching nearly all GP practices, with other regions to follow. In each region they have trained three GPs to become the regional expert with respect to antibiotics, and these people are responsible for providing the training and helping practices with their data extractions and calculating their outcomes of the quality indicators.
Speaking of her GRIP activities, Dr van der Velden was invited to be a keynote speaker at the Urgent Care Association (USA) annual conference and to present a webinar for members of the Urgent Care Association. The congress included a round table and workshop discussion where Dr van der Velden spoke with Lauri Hicks of the Centers for Disease Control and Prevention (CDC). Ms Hicks has fostered CDC, European Union, and World Health Organization collaboration leading to joint antibiotic awareness observances across several countries across the globe.
Dr van der Velden ended her update with a project that represents the majority of all the work she is doing currently. This is the coordination of the European Primary Care Research Network, which last year published their first large trial in The Lancet. This research network is continuing through the VALUE-Dx project running in Europe. It addresses the value of new diagnostics to appropriate antibiotic prescribing for community-acquired acute respiratory tract infection. She said, “Once again, we are working in a large European consortium in which our work includes clinical studies. At the beginning of this year we did a point prevalence audit survey registering in 20 European countries the clinical presentation and management of community acquired acute RTI”, she continued, “What we register from all these patients is how they present, what kind of comorbidities they have, what the GP’s management is with respect to diagnostics, whether they prescribe an antibiotic and if yes, which one, and what kind of over the counter medication do they advise.”
The aim is that in the end, information will be gathered on how physicians in these types of care settings manage patients with acute RTI across many European countries. Dr van der Velden added, “It also helps us to design a trial in the winter seasons of 2020-2022, introducing point of care diagnostics in primary care with the aim to reduce antibiotic use but not at the expense of patient outcomes”.
In addition to the usual European countries, data has also been gathered from Ukraine, Moldova, Armenia, Georgia and Israel, Dr van der Velden expressed her delight, “So that’s really exciting to see how healthcare works there and how motivated GPs are in collaborating”.
