Behaviour
Behaviour
The 5Ps Framework for the Non-Antibiotic Management of URTIs Progress and Challenges
The pentagonal 5Ps framework was developed by GRIP as an interlinking, flexible framework to highlight key areas of focus for antibiotic stewardship. The guiding principles include identifying patient attitudes to URTIs, educating HCPs on the appropriate management of URTIs and limiting antibiotic use to high-risk patients with bacterial infections, and establishing local policy for symptomatic relief of URTI. Local activations of global initiatives was the focus of 2015; targeting pharmacy, prescribers and patients.
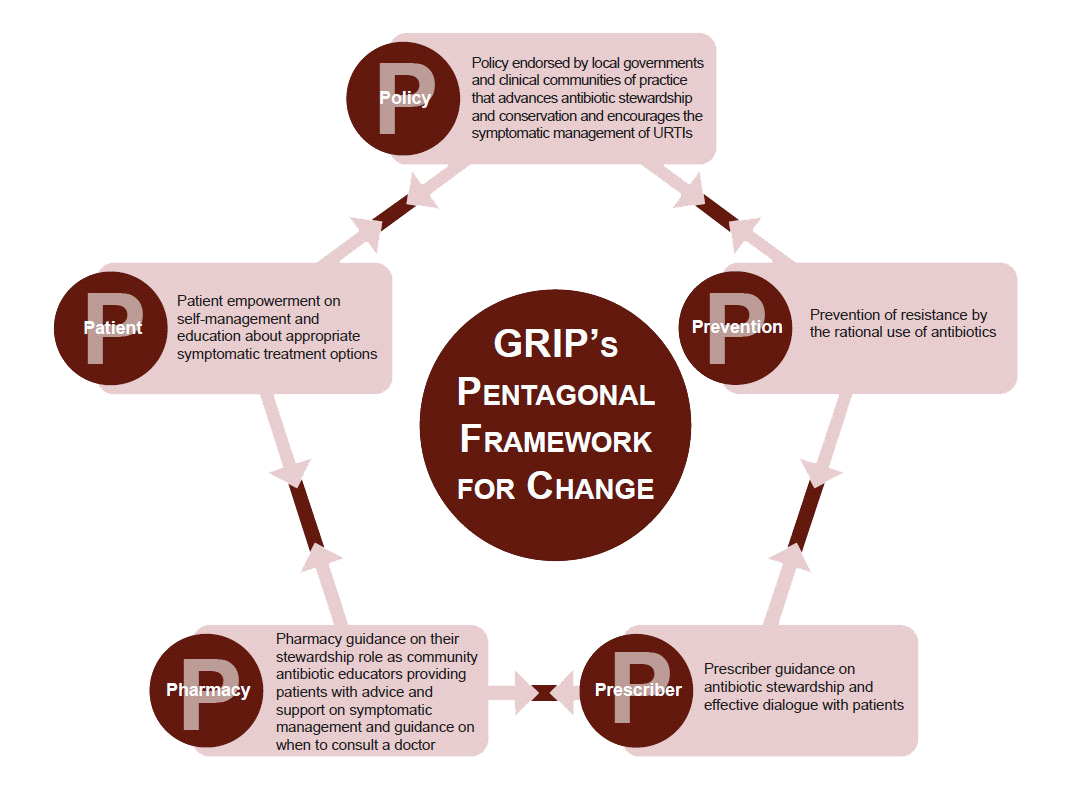
The GRIP’s pentagonal framework for change encompasses five key areas –Policy, Prevention, Prescriber, Pharmacy and Patient.
Pharmacy
The role of pharmacy is critical in promoting antibiotic stewardship. This is especially true for URTIs for which many effective symptomatic treatments exist. Pharmacists are strategically placed to educate patients and are therefore able to facilitate behaviour change and manage patient expectations in terms of demand for antibiotics. Pharmacists can help prevent AMR by impacting on prescriber practice and policy implementation. For these reasons, pharmacy should play a leadership and networking role among other organisations, in advancing a consolidated approach to AMR by antibiotic stewardship, specifically in URTIs.
Challenges and opportunities:
- In some countries, the role of pharmacy in antibiotic stewardship is embedded into national policy work, however even more needs to be done to highlight the value of the role of pharmacy to policy-makers
- There is a need to continue to empower pharmacists to have effective consultations with patients, in order to recommend more appropriate symptomatic relief treatments
Prescriber
Prescribers are vital in reducing the rates of antibiotic use for the management of URTIs. Prescribers can highlight the importance of self-management of symptoms and communicate realistic expectations of symptom duration. It is important that prescribers are able to recognise what patients actually want in the consultation rather than assuming the patient wants an antibiotic. Furthermore, they should explain why antibiotics are often not needed and recommend the most appropriate treatment.
Challenges and opportunities:
- Prescribers have an important role to play in highlighting when antibiotics are appropriate and when not
- An integrated approach to appropriate prescribing is needed
- Increased dialogue and understanding between pharmacy and prescribers will empower pharmacy to make recommendations; this enhances proper referral to each other
Patient
Patients are consciously and unconsciously able to pressure prescribers for an antibiotic prescription and are therefore a necessary focus for appropriate management of URTIs. Patients are often misunderstood by HCPs, who think they are seeking an antibiotic prescription, whereas they are often simply seeking reassurance and advice on how to manage their symptoms. It is important to educate patients on typical duration of symptoms, why antibiotics are not effective to treat the majority of URTIs, and highlight that there are side effects associated with antibiotic use.
Challenges and opportunities:
- Many patients still believe that antibiotics can prevent colds from developing into a more serious illness or help speed up recovery
- Patients seem to underestimate the typical symptom duration and when their symptoms last longer than expected they assume that they have something more serious than a URTI
- Often when patients deem they are ill enough to visit an HCP, they expect to be prescribed antibiotics
Policy
Policy varies both locally and globally, and while approaches need to be tailored per region there is also a need for consistency. Guidance needs to be put in place that advocates antibiotic stewardship. However, there is also a need for other measures that ensure the global alignment of policy, including: guidelines that discourage inappropriate use, HCP education and financial incentives to avoid the use of antibiotics for URTI.
Challenges and opportunities:
- While there is much guidance available on tackling AMR, this adds to the confusion – meaning that implementation of national or global guidance can be challenging
- There is a need for collaboration across healthcare settings to share consistent messages, learnings and experiences and develop local networks to ensure alignment
- Incentives that promote the stewardship of antibiotics should be introduced
- The effectiveness of selling OTC antibiotics for URTIs needs to be assessed in order for policy to be developed that aids antimicrobial stewardship
- Evaluation of effectiveness of regional interventions is important via review of rates and trends of antibiotic prescribing and resistance
- Efforts also need to be placed on patient and HCP education to support implementation of policy
